What is the perception of the EU in EU-AU partnerships
On the occasion of the European Commission Directorate for International Partnership A (Sub-Saharan Africa)’s away day, June 2023, I was invited as the Guest Speaker.
In view of the Global Gateway launched in 2022 as a point of departure for a new alliance between the EU and Africa. I was tasked with sharing an opinion with the Directorate A on the following: How is the EU perceived in partnerships with Africa? and What are the key challenges the EU can expect in project implementation?
As I was allocated a total of 1 hour, starting with a 15 minute speech followed by a Q&A session, I thought it wise to begin with a story about myself and provide context as to why I was there that day. I shared a picture of myself in Cameroon, 1997 at the tender age of 5 alongside a profile feature by the Africa-Europe Foundation on International Women’s Day, March 2023. To this, I shared that I had lived in Africa for 15 years and now in Europe for 16 years. I highlighted the internal conflict that often surfaces when the follow up to questions about speaking on Europe-Africa partnerships is usually along the lines of ‘which continent are you speaking on behalf of’. To be clear, I consider both continents home. After battling with this internal turmoil and posing the question to someone I consider a mentor – Baroness Estelle Morris, she said ‘Elsa you are a bridge and for a bridge to work, you cannot let go of either side. So, you have to hold on to both and try to be fair.’ I then stated, that is what I have done my entire life and that is what I would attempt to do today.
As a thriving millennial who considers herself on the pulse of new technology, it was inevitable that with the current scramble for AI and how topical it is, I turned to ChatGPT and Bard out of curiosity to answer the team’s pressing questions highlighted above. These were the answers I received:
It ended by highlighting that the overall sentiment was positive but there was room for improvement. As we know, AI tools are just that, tools, but very advanced tools. As a result, because of my knowledge in this space and work over the years, these sentiments are aligned with sentiments I have heard over the years. However, as the researcher that I am, I was curious to know what the sources of these information were. So, I went on to ask a further prompt:
Prompt: What are the sources of these information?
Answers: European Commission, The African Union, The United Nations, Academic Research
At this point, I felt the results may be biased by sources being large Governmental organisations. This also highlights key considerations when reviewing data on which Artificial Intelligence (AI) tools are trained. Therefore, I went on to use social media listening tools to scrape the internet and see what information was present from other grassroot organisations. I then came across a blog article written by Development Reimagined, an African led, Female led consultancy helping organisations and businesses to reimagine their approach to trade, aid, finance, climate action and much more. A snippet of the blog here:
To this point, the skeptical perceptions of the EU in these partnerships appear to stem from a lack of trust, lack of transparent communication, lack of trust in the EU’s motives and the EU’s willingness to execute on its promises (past).
While the drivers for these feelings appear to be numerous, an obvious comparison was that between the EU and China’s development work in Africa. I ensued to conduct a quick competitive intelligence on the type of development work the EU and China engaged in. This showed that among the flagship programs highlights by the EU, over 85% could be themed under the Sustainable Development Goals attributed to planet and prosperity. On the contrary, through a survey carried out by Development Reimagined where African ambassadors were asked where China’s contribution fall, the top 4 named SDGs were: SDG 1- No Poverty, SDG3 – Good Health and Wellbeing, SDG8 – Decent work and economic growth and SDG9 – Industry, Innovation and Infrastructure. This then begs the question that, does the type of work the EU funds and engages in affects its perception? And if yes, is this positively or negatively? Furthermore, how does the approach implored by funding partners such as the EU or China in building and maintaining relationships with implementing partners affect its perception? Does the EU gain enough visibility in this process? And overall, how does this affect trust in the EU’s motives?
Research conducted by SökerData Ltd on the level of trust between black and ethnic minority communities and Governmental institutions in the UK highlighted a 26% decrease in trust in comparison to pre-pandemic levels. Similarly, a study conducted by Mo-Ibrahim foundation across 34 countries highlighted a higher percentage of trust in religious leaders (69.4%) compared to local Government council (43.2%). This suggests that Governmental organisations or organisations that partner and work with Governments will experience a similar decrease in trust. Thereby, imploring these organisations to think about creative strategies to rebuild trust and engage with these communities.
To this end, building trust and engaging with these communities and countries, will entail strategies that cause organisations to reflect and review internal processes. This will include ensuring there is a high degree of co-creation with partners, the use of language that is inclusive for example swapping terminology like ‘hard to reach’ to ‘easy to ignore’. This will require transparency and accountability in the information shared and lastly building trust in a bottom up approach by engaging grassroot organisations and building trust champions for example with religious leaders who have a high level of trust. These are all attributes of an organisations’ culture, that is developed and implemented by its leadership and subsequently its people.
After spending half the day with the team, I truly left feeling there are absolutely good intentions, motives and the will to positively develop EU-AU partnerships. However, there are systems and processes in place that need to be reviewed so that these intentions can be translated, scaled and felt on a grass-root level. Considering this conversation was instigated by the EU team, it is a great step and sign of willingness to build a mutually beneficial partnership and I am hopeful this will materialise. As the implementation of the Global Gateway programs ensues, I look forward to seeing how trust is built in a sustainable manner while successfully delivering these programs.
Reaching 70% vaccination rate in the global south, would require creative, quick thinking and urgent action
The Africa-Europe Foundation announced a call for youth to contribute on specific topics about the relationship and types of partnerships between the continents Africa and Europe ahead of the AU-EU Summit. This contest was to engage youth interested in exchanges between the two continents and who want to work towards building a renewed partnership. Considering my background in Infectious Diseases and Global Health, I decided to speak on reaching vaccine access and equity in countries in Africa which currently have between 11-13% vaccination rates compared to 80%+ vaccination rates in the global North. My contribution focused on short term goals such as the urgency with which we as an international community need to reach 70% vaccination rate of the population in Africa and longer term goals such as creating Biotech ecosystems equipped for R&D. I won this call for contribution and joined the Africa-Europe Delegation for the AU-EU Summit albeit being virtual.
A couple of weeks after this, I was made aware of the “Forum Europe Afrique” where the Africa-Europe Foundation will be participating in partnership with La Tribune and La Tribune Afrique. It took place at the Palais du Pharo on March 17 in Marseille, France officially under the patronage of President Macron as a follow-up to the EU-AU Summit. Following my contribution, the AEF invited me to be a speaker on the panel on ‘Vaccination et Traitement pour Tous”. It was animated by Philippe Mabille – Directeur de la Redaction – La Tribune and speakers included:
Stéphane BANCEL : CEO and Chairman, Moderna Therapeutics (VIDEO) (could not attend), Philippe DOUSTE-BLAZY : President of UNITLIFE and former Minister of Health, Souad ABDERRAHIM : Mayor of Tunisia, Vice-President of the AIMF, Chrysoula Zacharopoulou : Member of the European Parliament (could not attend), Alan DONNELLY - President of the G20 Health & Development (zoom), Stavros NICOLAOU - Director of Strategic Business of Aspen Pharmacare and Elsa ZEKENG - Scientist, Entrepreneur, Activist
The panel debate started off with Philippe Mabille setting the stage and context for this debate followed by my contribution. I stated that when we talk about vaccines and treatments to which I’ll add diagnostics, I view them as public health goods/tools utilised in public health campaigns at higher rates during an epidemic or pandemic. I may go as far as saying in a pandemic, their level of importance and access to these is on the same level as basic human rights. If these are public health goods are essentially basic human rights, how did we get to a point where only a select few mostly in the global North have access to it. However, it is not a surprise as this has been seen before. During the HIV/AIDS pandemic, over a period of 10 years, over 12 million Africans died from HIV/AIDS out of lack of Access to Anti-retroviral drugs. Simultaneously, there was a drastic reduction in deaths from HIV/AIDS in the global North in countries like the USA.
When the biggest Ebola outbreak happened in West Africa between 2014-2016, there was a heavy reliance on support from the global North to increase access to these public health goods. Funding into Ebola and Marburg research over the period of about 10 years was about $1billion; of which almost 50% was given in 2014 & 2015. There was solidarity and collaboration with scientists deploying for knowledge transfer. A response, I was part of with the WHO and the European Mobile Laboratory (EMLab). As the COVID-19 pandemic ensued, we saw nationalism and individualism take front stage; where countries in the global south wanted to purchase these public health goods, but couldn’t. We saw and continue to see disputes of Intellectual Property, high cost, and exclusivity with access to public health goods where high-income countries received preference and access to these public health goods.
As we observe the patterns, this is not the first time this is happening. This cycle will be perpetuated if we don’t address the inequities in access to public health goods. Additionally, we need to create systems that can absorb epidemics and pandemics, move from a disease centred approach where during an epidemic and/or pandemic there is not a significant reduction in access to health care facilities and treatment for other diseases.
As we are a few days away from the fourth month of 2022, and review the target set by the WHO to reach 70% vaccination rate of the African population by mid 2022, the limited action to achieve this brings into question if this target is attainable. Taking into context the fact that some studies show the omicron variant could have been as a result of COVID19, staying and mutating in someone who was immunocompromised and likely unvaccinated. The implication of this is that the longer everyone isn’t vaccinated, the higher the chances of a new mutation and with globalisation, higher chances of another wave. It is therefore in everybody's best interest to meet this target. We need to think creatively, quickly and act urgently. We need to consider innovative Non-Traditional Partnerships with both old and new partners as well as create unconventional funding models.
As I stated on the panel (snippet below), some companies such as Moderna Therapeutics received more than $1 billion in funding for vaccine research funded by tax payers and then governments purchased these vaccines; essentially the business and shareholders have benefitted twice. Using public funds for research and development (including developing a vaccine), is a very common practice and one I totally support. However, I think it is only fair that in a situation such as a pandemic, the corporate takes responsibility to find innovative ways to support the public at large with access to these public health goods perhaps through Corporate Social Responsibility. Moderna stated it will not enforce COVID-19 patents while that decision is appreciated, without the knowledge transfer of vaccine development, this still delays mass production of vaccines. Afrigen Biologics in South Africa has been able to copy Moderna’s COVID vaccine with support from scientists in the international scientific community which will hopefully be on its way to clinical trial development and eventual manufacture. While this is promising, the time to delivery on these vaccines is still lengthy. Therefore, there is still the urgency to be met to vaccinate 70% of the population not just in African countries but also globally.
2 years into the COVID19 pandemic, the fight for vaccine equity continues..
Among many things, achieving vaccine equity through renewed partnerships between Europe and Africa will require sustained investment, investment in workforce capacity building, building research universities capacity and partnership distribution.
On Thursday last week, I was invited to participate in the Africa-Europe Foundation high-level special dialogue on Addressing the Vaccine Challenge for a renewed Africa-Europe partnership ahead of the 6th Africa-Europe Summit. I was (still am) absolutely honoured to have been able to listen in on such a crucial and important topic with leaders leading the charge on the African continent from WHO, Africa CDC to name a few as well as those from the EU; who are all committed to equitable access to health for all. This debate was very timely and looked at several factors at play in the access to equitable health for all in the context of COVID19 vaccinations. As I listened to the vital points being raised, while it was encouraging to see this conversation occur, it was also bittersweet as personally, it felt like ‘similar challenges, different disease, epidemic, outbreak or now pandemic’.
To provide some context, in 2016, I was selected as European Development Day young leader where I debated on high level panel organised by Politico about achieving sustainable healthcare with the decision makers such as Mark Dybul, then Executive Director of Global Fund, Martin Seychell, then Deputy Director General DG SANTE, European Commission and other highly esteemed leaders. Having deployed to Guinea during the biggest Ebola outbreak in West Africa with the World Health Organisation and the European Mobile Laboratory, I shared my experiences from working on ground. As part of the lessons learnt, we talked about the need for health system strengthening, equal partnerships and local capacity development. I questioned if we as a collective are actually learning the lessons from epidemics and pandemics to ensure we are more proactive rather than reactionary.
Elsa Zekeng, Young Leader, European Development Days 2016, Mark Dybul, then Executive Director, The Global Fund, Ronald de Jong, then Executive Vice-President and Chief Market Leader, Royal Phillips, Martin Seychell, then Deputy Director General DG SANTE, European Commission, Christiaan Rebergen, then Deputy Director for International Cooperation, Ministry of Foreign Affairs, The Netherlands, Martha Rojas-Urrego, then Head of Global Advocacy, Care International, Bob Collymore, then CEO Safaricom, Moderator, Ryan Heath, then Senior EU Correspondent and Associate Editor, POLITICO
During this debate, this sentiment was reverberated by Dr. Matshidiso Moeti – WHO regional Director for Africa as she stated that she was encouraged by this conversation and the investment and pledges being made to reach vaccine equity on the continent. However, she also stated, that as a continent, Africa has gone through several outbreaks and it was not so long ago that these conversations were occurring with regards to HIV/AIDS when patients were unable to access ARVs and positive outcomes emerged. Similarly, after the Ebola outbreak, there was a global movement from a global health security vantage point to establish a response. She stated, all the investment is deeply appreciated but this is a time of crisis, she hopes (I believe this is all of our hope) that we can reach a place where we demonstrate equity, investment and solidarity in times of peace and not just in a pandemic. She continued “We hope that the next crisis will find these investments have been sustained so Africa is found in a better situation and our health systems can contain the impact of an outbreak and continual delivery of services”. Hearing this, I definitely felt comforted but also reminded that achieving equitable partnerships and access to healthcare is truly a marathon and not a sprint considering Dr. Matshidiso Moeti has been in this sector for the better part of 20 years.
As the debate ensued, Pascal Lamy, a trustee from friends of Europe asked thought-provoking questions on if the lack of trust from Africa towards Europe had changed as well as what the status was on the bottle necks that have prevented fair access to vaccines on the African continent. These questions were very welcomed and appreciated by all and vocalised by Dr. Mo Ibrahim as he thanked Pascal for taking this conversation past political correctness and politeness. Dr. Raji Tajudeen – Head of Africa CDC public health institute and research responded to Pascal’s questions highlighting that yes, Africa felt let down as once again we saw nationalism at play, not just in terms of vaccines but also other medical supplies. He provided context to the challenges faced on the African continent stating that “there are 1.2-1.3 billion people in Africa, to get to WHO target of 70% COVID19 vaccine coverage, we need to immunise around 900 million people, through COVAX, we have 350 million vaccines, through the Harvard mechanism we have 400 million vaccines. In terms of supply, we aren’t doing badly. However, what is the point of vaccines if they aren’t getting into people’s arms. The greatest challenge is delivery, last mile delivery on one hand and creating the necessary demand for people to take the shots.” Additionally, he shared that CDC Africa and London School of Hygiene and Tropical Medicine conducted a multinational arm survey in late 2020 which was repeated 3-4 months ago and it showed 4 out of 5 Africans were ready to take these vaccines. Of the 20% who were unsure, it was not necessarily a case of anti-vaxxers but more so the need for more information.
Average acceptance of the COVID-19 vaccine across studies and subgroups within studies. The average acceptance rate across the full set of LMIC studies is 80.3% (95% confidence interval (CI) 74.9–85.6%).
One of the main challenges raised during this debate was the fact that many vaccines arriving on the continent were close to their expiry date making it almost impossible for countries with already limited resources and mechanisms to deploy these fast enough for use. This led to the release of the joint statement from WHO, GAVI, UNICEF, CEPI, African Union, African CDC requesting all vaccines being donated to Africa need to have a minimum of 10 week shelf life when they arrive on the continent among other things. Ashleigh Furlong, a journalist from politico questioned if this had a part to play in vaccine hesitancy as citizens could feel they were getting vaccines ‘Europe doesn’t want”. Dr. Raji Tajudeen commented on this stating that vaccine hesitancy is multifactorial and underpinning this is a lack of adequate information. Dr. Mo Ibrahim echoed these sentiments but also highlighted that hesitancy is a global phenomenon and not an African one as this was evident in Austria, Switzerland, USA and many other countries. It has more to do with us as human beings, misinformation or disinformation. He went on to state that the challenges being faced are not a result of a lack of ‘knowledge on what to do” but rather the angle the political landscape brings. Several pledges were made in 2020 from several world leaders coining the phrase – “nobody is safe until we are all safe”. We all used that phrase, including myself in May 2021 as I wrote about vaccine equity. However, several of these pledges seem to have fallen through the cracks as we continue this conversation 2 years on.
European Commissioner for International partnerships, Ms Jutta Urpilainen responded admitting that yes there is a still a lot to be done but also defended the EU politicians stating that in terms of donations and financial support, the EU has led the efforts within the international community to assist African countries to attain vaccine equity. This solidarity led to founding COVAX and so far, 1.45 billion vaccines have been exported to Africa. She continued highlighting that out of €46 billion contributed to help 146 countries cope with the pandemic, €10 billion has gone to Africa. She stated that the EU has committed to share at least 700 million doses by mid 2022, about half of the vaccines donated has reached Africa. However, we know donating vaccines is just one part of the challenge while ensuring they make it to people’s arms is the other. She emphasised that in the short term, the EU will continue to support the urgent response to COVID19 including vaccine deployment as €100 million has been contributed to support vaccine deployment in Africa. This will have a dedicated vaccine support package to roll out at country level.
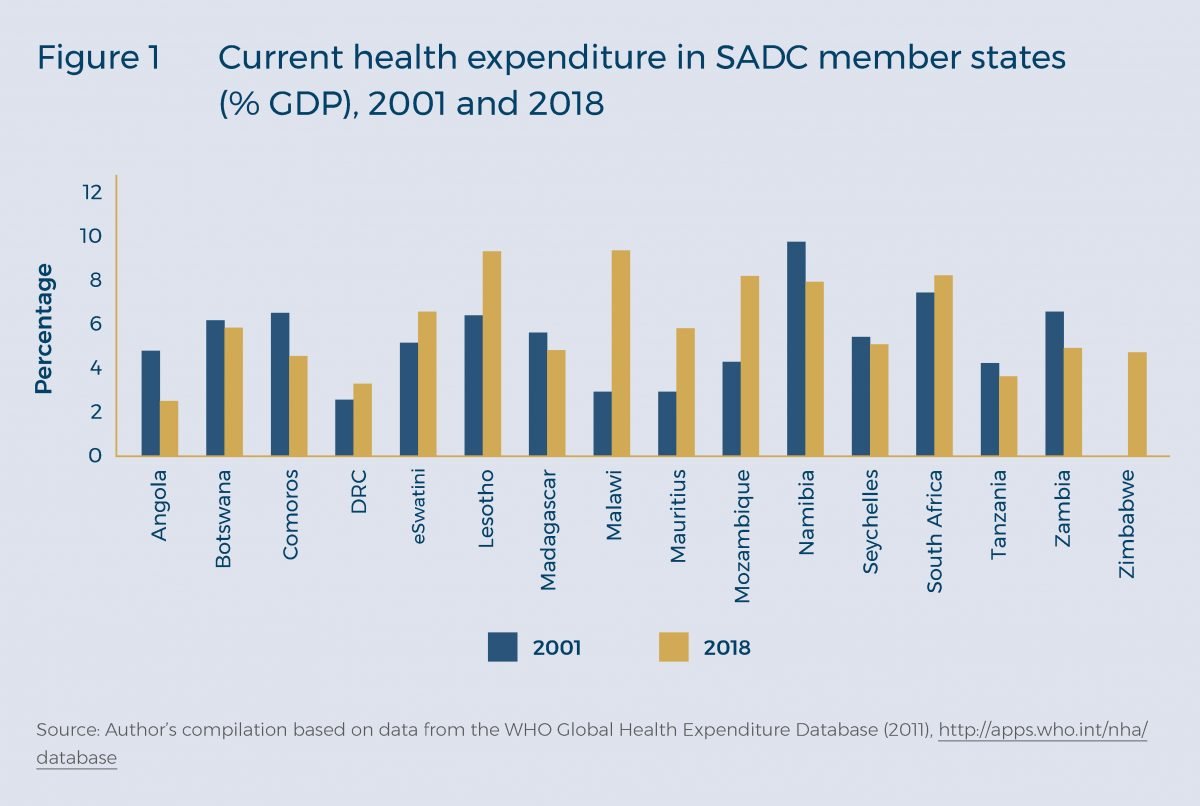
Dr. Mo Ibrahim returned the accountability to Africa stating that Africans have made mistakes, the health systems are weak and so is data collection and countries need to strengthen their Office for National Statistics. When we review the Abuja declaration, the spend agreed on the health sector was 15% of their annual budget, however, countries average between 6-8% spend. This has improved over the years but is still not in accordance with what was agreed in many years ago. Therefore, African countries have a lot of adjustments to make in-country before blaming anyone else.
A snapshot of health expenditure from countries in the Southern African Development Community (SADC)
As the AU-EU partnership seeks sustainable solutions to arrive vaccine equity, a critical component is development of vaccines on the African continent to allow for capacity building and quicker vaccine deployment. Dr. Marie-Paule Kieny highlighted the importance of local production of vaccines on the African continent owned by African government with technology free of rights to produce not only COVID vaccines but HIV, TB and any other infectious diseases. She stated that Afrigen in South Africa will develop the technology and transfer this to multiple partners (to be announced by Dr. Tedros Adhanom, Director General of the World Health Organisation). Dr. Morena Makhoana, CEO of Biovac highlighted the importance of the private sector as a stakeholder, the importance of looking at Africa as an equal partner, the need to have a market that is sustainable to keep Africa alive and this requires sustained investment accompanied by the right technologies and capabilities. This was supported by input from Dr. Sierk Poetting, COO of BioNTech stating their support to Senegal, Rwanda and South Africa for the construction of decentralised end to end manufacturing network and building local capacity for mRNA through transfer of knowledge. All these points were supported by Martin Seychell, Deputy Director General at DG International Partnerships - European Commission, stating that the business case for Africa to have a vaccine development hub is clear but we need to ensure that the support from partners is leveraged, human resource is built, the ecosystem is de-risked to encourage further investment and pharmaceutical research is supported, as it is from research that entrepreneurship flows.
This debate was moderated ever so gracefully and efficiently by Tamsin Rose, senior fellow for health at the Africa-Europe foundation who finalised the take home messages in the following points; the need for sustained investment, investment in workforce capacity building, building research universities capacity and partnership distribution and clarifying the Africa – Europe direction. In closing, Chrysoula Zacharopoulou, a member of the European parliament and gynaecologist stated that we need to invest in Africa, firstly through the 15% of public finance that was pledged by African Heads of states in the Abuja declaration. Additionally, implementing manufacturing, regulations and mechanisms in partnership with the international community is equally important. However, pushing back on Dr. Mo Ibrahim’s stance on vaccine hesitancy, she stated that in her experience vaccine hesitancy is cultural and trickled into belief systems. She stated that in this renewed partnership, Africa has a role to play in taking care of its citizens and Europe can accompany and support.
This debate was clearly one that is timely and essential to encourage and sustain equal EU-AU partnerships. However, these conversations occur after a crisis as Dr. Matshidiso Moeti stated and we hope these investments are sustained to meet the next crisis. As we continue these conversations for renewed AU-EU partnerships, it is essential that the youth are brought in to participate to understand the historical context of these exchanges following outbreaks from HIV/AIDS to Ebola and now COVID19. Participation that isn’t limited to one event but rather ensuring continuity so that there is increased awareness, preparedness and continued partnership building. In the last 7 years, I have participated in the response to the Ebola outbreak in West Africa and in discussions around changes to be implemented. During this time, I also completed my PhD in Infectious Diseases and Global Health and have keenly followed the COVID19 outbreak; from the science and research, to public perception and attempting to understand human behaviour in unprecedented situations and of course the response from pharmaceutical companies and the interplay between politics and public health. While my eagerness and somewhat frustration makes me think we have had many of these conversations before and noted the lessons learnt, I have to acknowledge that there has been progress but there is more we could have done and can do. I recognise the time and effort it takes to move the needle towards implementing sustained change in our health systems and renew partnerships. This led me to the thought that there needs to be a continuous intergenerational ‘passing of the baton’ and involvement of youth at every stage to provide an understanding and context on what has been done and what still needs to be done. Additionally, investing in ecosystems that are fast growing for example biotech start-up ecosystems in Africa is imperative. The benefits of start-ups include their agility and ability to be more iterative to arrive at quicker solutions in the face of unprecedented situations. Finally, in the short term, these partnerships should include engaging with new partners in the private sector who have the technical knowledge and logistical bandwidth to support in addressing some of these bottlenecks.
COVID19: “Either we are all saved or no one is safe”
If you are reading this and you are based in the United Kingdom, I think I am right in speculating that you currently feel some sense of relief, excitement, anxiety or all of the above as we step in phase 3 of the roadmap out of lockdown. A lockdown that our Prime Minister announced on the 23rd of March 2020 stating the “UK can turn the tide of coronavirus in 12 weeks”. Well, it only lasted 1 year 1 month and 3 weeks and will be continually reviewed; we aren’t out of the woods yet. So, yes, phase 3! I am looking forward to indoor seating in restaurants (I am not committed enough to eat out in the cold) and I am excited to regain access to the hot yoga studio!
We have experienced 3 national lockdowns, various restrictions in the form of tier systems and several public health measures including the vaccine campaign. We’ve stayed home, shielded, isolated, mass tested, and most recently seen the roll out of the vaccinations. As it stands, in the UK, more than 33 million people have had their first dose of the vaccine and eight million have had their second vaccination. A single dose of the vaccine can reduce household transmission of the virus by up to half.
Some of these measures have been met with both compliance and scepticism. A direct outcome of compliance can be seen as 50% of the UK population is now vaccinated. We have also seen resistance in the form of lockdown protests. Research carried out to attempt to understand compliance or non-compliance to public health measures has been segmented by ethnicity, level of education and even employment status. This research has shown and suggested that black and ethnic minority communities are least likely to take the vaccine in comparison to white communities. However, this rate has fallen from 44% (13 January to 7 February) to 22% (17 February to 14 March).
It is key to remember here that in any uncertain situation, a pandemic being an example of one, trust plays the biggest role in compliance to a set out strategy – this includes public health measures. Trust in the motives of the Government and trust in science and the staff developing vaccines and generally advising on these measures. Research conducted by the London School of Hygiene and Tropical Medicine in April 2020 showed that 52% of respondents thought the Government were doing a good job to control the spread of the pandemic. Out of 9000 respondents to this survey, there was a very low response from black and minority ethnic communities. This shows that the scepticism goes across ethnicity lines. Notwithstanding, black communities have a history of mistrust with the Government (lived experiences of slavery) and the scientific communities (unethical medical practices).
While in the UK, we feel some sense of relief, unfortunately, this feeling is not global. Just 2 weeks ago, India recorded more than 300,000 positive tests each day for a week. Medical supplies are being shipped from 15 countries, estimations suggest India would need about 500,000 ICU beds and 350,000 medical staff in the next few weeks. This is a stark difference compared to the current 90,000 ICU beds it has that is almost fully occupied. We can explore all the reasons why there is this second surge and critique what has been done or left undone but now is not the time. What we need to focus on is what can be done now. Countries like India do not have the same privilege to put in place the types of public health measures that the UK has, especially in terms of vaccine roll out.
Just to be clear, this article is not to debate the efficiency of vaccines including the COVID-19 vaccine (I’ll focus on this in another article). However, it is worth stating that as a scientist with a PhD in infectious diseases and global health, I am pro-vaccines and believe in vaccine rollout as a public health measure. Rather, my hope is that, this article highlights the inequities in public health measures such as vaccine rollouts and challenge us to think about sustainable ways of addressing these.
Israel is leading the charge in terms of vaccine roll out with 62% of its population vaccinated, followed by the UK with 52% compared to India that has vaccinated 10% of its population. Access to vaccines is a privilege and affected by various factors primarily finance. The patents of the vaccines against COVID-19 developed by private pharmaceutical companies such as Pfizer and AstraZeneca to name a few has made it difficult to produce more and roll out to other countries specifically developing countries. The Biden administration released a statement in support of the release of patents, this has been supported by Spain and in accordance with other countries such as India and South Africa. Unfortunately, this has been met with resistance from pharmaceutical companies as well as Germany rejecting this push to waive COVID vaccine patents.
While I understand the need to protect intellectual property, right now, this feels like greed. There is a challenge and there is a solution but only some people have access to this solution – that is the definition of inequality. The impact of COVID19 as we know go beyond our individual health, the longer it lasts, the longer economies suffer, the more limited access to opportunities etc.
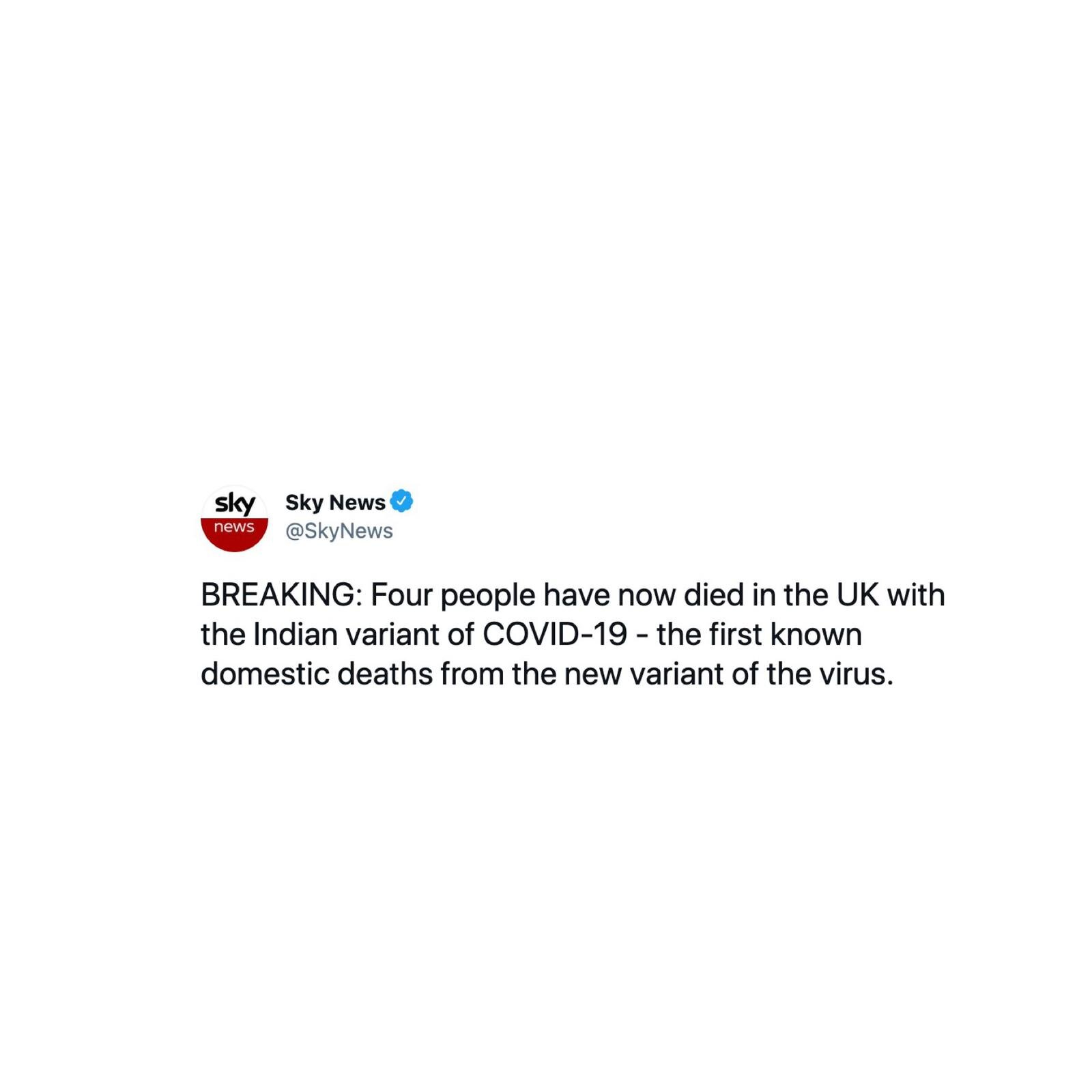
Furthermore, in this interconnected world, none of us are safe until all of us are safe. This can already be seen as sky news announced four people have now died in the UK with the Indian variant of COVID-19.
As we debate on the way forward, we need to remember that the balance of power (that includes economic power) between high income countries and low-income countries affects every single outcome including health. Delaying to act only widens the gap. When we think about strategy, we need to remember that while there are several initiatives raising funds for the provision of the vaccines for example the Global citizen concert COVAX live, there is also a cost (approximately $1.5 per dose) associated with rolling out the vaccine which is usually not accounted for or underestimated. As we, the lucky ones be it as a result of being geographically based in a country that has access to finance, vaccines and healthcare, take a deep breath and wish the pandemic away, let’s remember there will be another epidemic or pandemic and we still are not prepared. We rewrite the same lessons from past epidemics but somehow, we fail to learn from these lessons and resist implementing the necessary change.
My hope is that:
1) We create a sustainable financial model accompanied by ethical laws that will see Intellectual property and lives protected in the face of such scenarios (a pandemic)
2) We create a sustainably financed World Health Organisation that is independent of national politics. We needed a global leader during the COVID19 pandemic and unfortunately, we didn’t have one.
Sending the most heartfelt condolences to the families of the 3,372,019 who have lost their lives to date as a result of the COVID19 pandemic
To be a woman in 2021
International Women’s Day 2021 is approaching. The requests to speak on panels are flooding in and the theme for this year - #ChooseToChallenge.
It is Monday March 8th 2021, social media is filled with posts stating Happy International Women’s day. We see pictures of several men and women with their right hand up “choosing to challenge”. While some take part, others question the meaning behind this. Is this just another hashtag? What is the action behind this?
Nonetheless, the pictures keep coming in – on my LinkedIn feed, I see people challenging systems to increase investment into start-ups and companies founded by women, on my Instagram feed, I see people challenging colorism and institutional racism, on my Twitter feed I see people some people just “choosing to challenge” and others stating they would miss out on this hashtag and continue to do the work which really is hiring more women and paying women equally.
At first glance, and with the amount of activity going on social media, one would think – we are in a revolution and people are truly choosing to challenge old systems and ways of doing things. Basically, a step towards true gender equality. Well, the events over the next few days, reminded me of the society we still live in, one that talks about change but truly isn’t ready for it. One that asks women to challenge until that challenge is too uncomfortable for them.
Well, on Monday March 8th at 9pm, the much talked about interview between Meghan, Duchess of Sussex, Prince Harry, The Duke of Sussex and Oprah was aired on ITV for the British public after airing on CBS in the United States the night before. On Tuesday 9th of March 202 morning, I alongside everyone watched as the interview was dissected by “experts”, fans and really anyone who cared about the Royals. To date, this interview had over 17 million live viewers on CBS, in the UK alone, it garnered a massive 11.3 million viewers and around the world a whopping 61 million people viewed the interview so of course everyone had an opinion.
Harry and Meghan spoke their truth and fairly intimate details. Meghan shared conversations that were had about “concerns over their son – Archie’s skin colour”. She even shared details of her mental health deteriorating to the point “she didn’t want to be alive anymore”. She talked about how she wanted help and unfortunately was not offered any. (I truly dropped a tear then). I can go on and on about so many bits that made me reflect on the society we currently live in. Let me first state – I am #TeamSussex all the way and I was not naïve to the fact that they would be met with much backlash especially knowing and living in the UK for over 10 years. I was however appalled by the disparaging comments made to the point Pierce Morgan stated he “didn’t believe” she was telling the truth about having suicidal thoughts. If you aren’t #TeamSussex for whatever reason, that is totally fine, we are all entitled to our own opinion. But, to say you think another human being is lying about having suicidal thoughts…what or who gives us the right to question someone’s mental state of being? Whether you are of the opinion that they (Harry & Meghan) were/are “spoilt brats” and Meghan was the mastermind manipulator and coerced Harry into this, at no point should we as a society ever come to a place where someone feels scared to share their struggles with mental health because they fear not being believed. We have seen this play out one too many times with the #metoomovement and that greatly affects victims’ willingness to step forward.
I couldn’t help but think, weren’t we all telling women to #choosetochallenge yesterday? *Very confused*
As I grappled with this, on Wednesday 9th March 2021, human remains found in Woodland in Ashford Kent were formally identified as Sarah Everard the 33-year old Marketing Executive who had gone missing 6 days prior. She went missing after leaving a friend’s house in Clapham, South London at around 9pm. She is believed to have walked through Clapham Common on her way home to Brixton, but she never made it. The scariest part was that a serving Metropolitan police office has been charged with kidnapping Sarah Everard from the street as she walked home and then murdering her.
There I am again thinking – What world do we live in? A reminder that as a woman walking home at night is a huge risk. You cross the streets when you hear footsteps behind you, you make sure your music is not too loud to ensure you’re still aware of your surroundings, you do not take short cuts through the parks or unlit alleys, you hold your keys in your hands, you pray with each step you take and you countdown till you’re home but most frighteningly, even at the hands of the police, you still are not safe!
It reminded me of Blessing Olusegun, the 21-year-old carer who never made it home but her body was found on a beach in East Sussex with her phone and slippers next to it in September 2020. Her death was deemed as “unexplained” by Sussex Police but no further investigations were made into this. Of course I start thinking about the intersection between race and gender. Sarah Everard’s case was solved in 9 DAYS, yet 5 months later, Blessing’s case is still “unexplained”.
On Thursday 10th of March, Caroline Flack’s mother – Christine Flack warned that the media has failed to learn the lessons of Caroline Flack’s death and must take responsibility for coverage of public figures struggling with mental health problems. Caroline Flack, a well-loved TV presenter passed away by committing suicide in February 2020. Again, this was another reminder of the fragility of life and to be more precise women.
On Saturday, a vigil for Sarah Everard was planned in London. Granted we are still in a pandemic and there are restrictions but nothing in my opinion calls for the level of violence we witnessed. The violence that saw a woman of about 5 foot 2 in height on the ground held in handcuffs by 3 male officers. The only thought that comes to mind is - where is this same energy for male offenders? Especially considering the culprit in question here is a fellow Metropolitan officer.
Here we are – Sunday 14th of March – its Mother’s Day and again my timeline is filled with loving pictures of their mums and appreciation for women.
This is where I get angry, disgusted and confused. All the women highlighted here, Meghan, Sarah, Blessing, Caroline Flack they were first and foremost women, then they are someone’s sister, mother, wife, best friend etc. How do we as a society truly say we support women, we want gender equality, women should challenge and speak up but at every chance, find a way to silence her – be it by bullying, harassing, blackmailing, gaslighting her, telling her she is saying too much, assassinating her character or worst still assassinating her…
I realise I am a very “black” or “white” person, you know - “hot” or “cold”. I truly despise the “grey” or “lukewarm” areas. So, I’ll rather feel like a society does or does not support gender equality so at least I know where I stand. As Trevor Noah frequently jokes, racism is South Africa was “better” because it was obvious – you had signs saying “white only” or “no blacks allowed”. Basically – you knew where you stood.
Unfortunately, this is not our reality. We live in a society filled with grey areas. Grey can be ok when you are talking about colour palettes to paint your house, BUT, when it comes to human life, when it comes to women’s life, her right to speak, her right to be included and heard, we cannot have Grey! No, it doesn’t work and in my opinion, it is worst because it gives a false sense of progress - it is frustrating and infuriating. This type of grey can truly cause someone their life! Let this week serve as a reminder of that – we are nowhere where we need to be as a society! We need more actions – less words!
Trends and Technologies sped up by COVID19 that are here to stay.
As a scientist, the concept of a pandemic is not all too novel. As a matter of fact, it is something we spend a lot of time thinking about – which virus would it be, what would be the origin, how would we test it, how would the public and policy react to it? We run simulations & prepare for the eventuality. Just to clarify, this is not because we spend our time in the lab creating mutations but rather we study it. Caveat here – that is not to say these viruses can’t be engineered or used as biochemical threats – but I think I speak for most scientists who have dedicated their lives to research when I say – we research viruses purely out of passion and our innate curiosity to understand mechanisms of action but more so the biology and molecular biology underpinning these changes. One thing that we know is everything changes – human nature changes, animals change, human beings evolve, so why would viruses not do that same thing? It is only logical. Look at the Influenza A Virus for example, it mutates yearly to escape our own body’s immune response to viral infection.
So here we are - February 2021, almost a year since the World Health Organisation officially declared COVID19 as a pandemic on the 11th of March 2020. Following this, we have seen and experienced different strategies from countries responding to the outbreak. As it stands today February 22nd 2021, according to the latest data from Statista on COVID19 deaths worldwide per one million population, the United States of America has the highest number of confirmed cases with 27,999,614 registered cases, the United Kingdom has 4,103,444 registered confirmed cases while China where the virus was first detected in December 2019 has 100,758 and Australia - 28,930 confirmed cases. This has all been as a result of the intersection of policies and healthcare. I will definitely explore this in more depth in another article.
However, today, I am focusing on the effects of COVID19 on society - the trends and the technologies that we have seen in the last 12 months. According to a McKinsey & Co report – COVID19 has accelerated 5-8 years of change in 1 year. Here are some trends I have particularly find interesting & I am excited for the future and prospects they brings:
1- Remote working:
Personally, this has been one of my favourites. I have always been an advocate for remote working, I have worked remotely pre-COVID19 and I have absolutely loved the autonomy and flexibility it gives. Being able to wake up slightly later, no commute hours, fitting in a workout in the morning, reduction in carbon emission (might as well address global warming while we are at it), “signing out of work” and having a bit more time in the evening for our families and so much more. I understand that this reality is different for parents who are home-schooling children and also not everybody can work remotely. However, if this is a possibility then definitely why not exploit it? I know there are other cons around this such as working longer hours due to not creating defined boundaries but also not creating work hours and work spaces boundaries. As with everything – change comes with adaptability; it is up to us as individuals to create new routines to thrive.
2- Video Conferencing:
“You’re on mute” was probably the statement most used in 2020 after the word “unprecedented”. I am sure we have probably had our fair share of video conferencing platforms be it Zoom or Microsoft Teams but we can agree it has allowed us to appreciate all the meetings and events that could have been held online. I would always be in support of face to face meetings and human contact but the normalisation of video conferencing greatly supports remote working but also gives us the ability to truly prioritise what needs to be a face to face meetings and what could be held online.
3- E-Commerce to V-Commerce:
We always knew the power of e-commerce nonetheless, prior to the pandemic, shopping online was a convenience and for some shops, a nice to have however, the pandemic made it a necessity. As evidenced by online giant Boohoo purchasing high street store – Debenhams for £55 million, Dorothy Perking, Burton & Wallis for £25 million and ASOS purchased Topshop, Topman and Miss Selfridge for £330 million. Taking it a step further, Anifa Mvuemba a Congolese designer staged a fashion show over Instagram Live, with 3D renderings in place of models. This takes the world of fashion, shopping, runway shows, catwalks to the next level. The opportunities for this in the future are endless – a potential reduction in model fees, the politics of “front row” seating at fashion shows and so much more. I look forward to seeing how this evolves.
4- Entrepreneurship & Career changes:
Another thing COVID19 has presented us with is a lot of time at home. Time to reflect on our families, careers and all round contentment & happiness in life. A recent report showed 53% of workers based in the United Kingdom plan to make career changes in the next 12 months. A lot more people are up skilling, retraining and/or starting businesses. Plato said it best – Necessity is the mother of invention. A McKinsey & Co report showed there were more than 1.5 million new business applications in the United States almost double the figure for the same period in 2019. While France saw 84,000 new business formations in October 2020, 20% more than in the same month in 2019 while in the United Kingdom, this rose to 30% in the third quarter of 2020 compared to 2019. I think one thing COVID19 has reminded us is that – life is short and fleeting, considering how much time we spend working, we need to ensure that we enjoy and love what we are doing. So if you have the entrepreneurial flare/curiosity, why not delve into it?
5- mRNA Vaccine:
Previously, vaccine development has focused on using inactivated or attenuated form of a virus to allow our bodies to develop an immune response to the viral infection. The concept of messenger RNA (mRNA) vaccines has been around since 1990 with researchers making it work in mice. Essentially, mRNA vaccines carry instructions that tell the cell exactly what protein to code for that would prompt an immune response. The mRNA is then broken down within 24 hours. These are the first vaccines to have secured regulatory approval. The benefits of mRNA vaccines are that they are made from sequencing a genetic code, this can be done in a lab within 48 hours, once you have this code and set of instructions, an experimental batch of vaccines can be produced even within a week. This means it can be standardised and scaled up pretty quickly which considering an epidemic or now pandemic, which is a case of public health emergency, this is a substantial benefit. Again, the nerd in me - is super excited for the future of bio-technology (another topic I will cover another day)!
Let me know your favourite COVID19-enhanced trends that you hope become permanent.
The chips are stacked against us women..but we continue to thrive!
As I contemplated the first blog post, I thought considering the “unprecedented” times we currently live in, it would be about the COVID19 pandemic. I put unprecedented in quotation marks because we have all heard that word one too many times over the past year. So I write it with a twinge of cringy-ness and a bit of an eye-roll.. Anyways, I digress… I considered the many things I wanted to explore about the COVID19 pandemic: from the development of vaccines, the administration of these vaccines, the different lockdown measures, the mental health effect, the inequities in those affected with a focus on black and ethnic minorities to an overall view on the importance of the space between science, health and policy for meaningful change. These are all topics I will definitely explore at some point in the near future but as I mulled over these topics, I was pulled in another direction with this headline news this last week.
So here I am, dedicating my first post to Whitney Wolfe Herd’s life journey.
In order to appreciate any story – positive or negative, it is imperative to have some context around it. Maybe it is the scientist in me who is always seeking facts and evidence but hey – Let us take it a step back and for context.
Bumble is a women-centric dating app where women make the first move in heterosexual relationships. Insights in to the app showed users are more likely to pay for premium offerings to have a deeper level of connection and browse others’ profile while being anonymous. She actually expanded this to Bumble BFF, where women can form friendships and Bumble Bizz to expand their professional networks. Considering I am writing this on Valentine’s Day 2021 – If you’re single and searching – you know what to do ;).
Here are five things to note about Whitney Wolfe Herd, the driving force behind Bumble..
1- She has a degree in International Studies from the Southern Methodist University
2- She actually co-founded the “Tinder” app, she says she came up with the name “Tinder”. She was vice president of marketing for Tinder and has been credited for fuelling its popularity on college campuses.
3- She dated fellow Tinder co-founder and then-boss – Justin Mateen. She was ousted from the company after they split. She filed a lawsuit for sexual harassment and discrimination which was settled outside of court and she netted just over $1 million plus stock from the settlement.
4- After enduring online hatred, she decided to rebuild herself and launched Bumble in 2014
5- At 31, she became the youngest female CEO to take a company public in the United States with over 70% of the members on Bumble’s board being women. The stock soared 64% in its Nasdaq debut making Wolfe Herd’s 21.5 million shares worth over $1 billion.
Since 2017, Bumble has had its unicorn distinction with the company’s valuation above $1 billion with investment from Andrey Andreev, Wolfe’s close friend and business partner– who owned 79% stake in Bumble. After allegations of sexism and racism, Andreev sold his stake in the business and was now worth $3 Billion.
Now, being a woman and entrepreneur in the Tech ecosystem, Wolfe’s story is an inspiration. According to data from PitchBook, female founders received 2.2% off $130 billion in VC funding in 2018. In 2019, Venture Capital investment in all-female founding teams hit $3.3 billion representing 2.8% of capital invested across the entire U.S Start-up ecosystem.
However, as an immigrant and black woman, with all the dreams, goals and work ethic in the world, while reading and writing about Wolfe’s story, inspired by it, there is still that all looming feeling of exasperation at the back of my mind – as I contemplate the intersectionality of gender and race and access to Venture Capital investment. Black and Latinx women combined, receive jut 0.64% of total venture capital investment between 2018 and 2019. 0.37% went to Black women and 0.37% went to Latinas.
Two things come to mind as I reflect about this especially in an era where several companies are pledging to diversity and inclusion, pledging to supporting black founders and female founders. In an era where the #metoomovement has taken several twists and turns;
1- Starting a tech company more often than not requires capital to truly make an impact. Access to this is minimal as a result of institutional and personal bias and a lack of “knowing the right person or someone willing to give you a warm introduction”. In the last 2 years, we saw companies such as Paystack founded in Nigeria by Shola Akinlade and Ezra Olubi that sold to Stripe for $200 Million and Tope Awotona founder of Calendly that recently received Unicorn status by receiving $350 Million in investment from OpenView Venture Partners valuing the company at $3 Billion. While that is encouraging, we need MORE! Black female founders cannot only have 0.37% of total Venture Capital investment. I am certain it’s not because of a lack of companies, ideas or entrepreneurs to invest in – but rather limited access.
2- As much as I truly dislike this thought - As a woman, why do the chips always seem to be stacked against us? Primarily, the obvious- access to finance and investment. More personally, in the event of a fall out especially in a romantic involvement as was with Wolfe’s story, more often than not, the woman receives the short end of the stick. She is called several names and her contribution undermined. I know, I know, you may be thinking – that is why you don’t mix business and pleasure - true..but why does the burden of shame and repercussions fall on the women even though both parties were involved? It’s the harsh reminder of – “This is a man’s world”. What is clear though is - should Wolfe not have filed a lawsuit against Tinder, she would have walked away with nothing!
Anyways, to all my women entrepreneurs out there, specifically like me from minority ethnic backgrounds, keep striving, keep believing, whatever situation you may find yourself in – fight your corner but make sure you bounce back. In the words of Amanda Gorman, “there is always light, if only we’re brave enough to see it, if only we’re brave enough to be it”.
Healthcare Systems in Sub-Saharan Africa
There exists a continuously growing health care gap between Africa and the rest of the world.
Abstract:
There exists a continuously growing health care gap between Africa and the rest of the world. Sub-Saharan Africa (SSA) accounts for 11% of the world’s population and bears 24% of the global disease burden. A total pipeline of up to $25-$30 billion is scheduled to be invested to address the need for healthcare assets such as hospitals, clinics and warehouse distribution in SSA. There have been major strides to alleviate the disease burden on the population of those affected as well as improve patient care. These have been limited to a number of Sub-Saharan African countries and therefore need to be implemented more widely within the region. Most importantly, more efficient strides need to be made towards investing in research institutes within the local community as well as the development of medical products. Promoting community-based delivery (CBD) of medication, health services and social work in tandem with the pre-existing healthcare system will go a long way to increasing access to health facilities. Not withstanding the need for revising and implementing policies for the greater gain of the public. There are high stakes involved including a very high level of commitment from various parties but this is not insurmountable.
Keywords: Research institutes, Sub-Saharan Africa (SSA), Community based delivery (CBD), health services, and medication
There exists a continuously growing health care gap between Africa and the rest of the world. Sub-Saharan Africa (SSA) accounts for 11% of the world’s population and bears 24% of the global disease burden. However, this percentage of the world accounts for less than 1% of the global health expenditure. Over the last decade, as part of a healthcare improvement regime, a significant amount of financial aid worth over $8 billion has been allocated to SSA. The rural inhabitants succumb to and are victims of poor health care facilities, personnel and access to medication (1, 2,3). The most recent and biggest Ebola outbreak in West Africa highlights the loop holes and failures of the healthcare systems in Sub Saharan Africa. While countries like Mali, Nigeria and Senegal successfully contained the disease; other countries like Guinea, Liberia and Sierra Leone relied heavily on foreign help. The eminent need for capacity building and capacity enablement are highlighted alongside the one-sided benefit of international aid for economic development of research collaboration to the donor rather than the recipient (10).
Despite the financial influx of capital from the international community, only a few countries in Sub-Saharan Africa are able to provide the minimum healthcare as defined by the World Health Organization (WHO) to be within the range of $34-$40 per person3 estimates suggest that over the next decade, a total pipeline of up to $25-$30 billion is scheduled to be invested to address the need for healthcare assets such as hospitals, clinics and warehouse distribution in SSA (1).
The Joint United Nations Program on HIV/Acquired Immune Deficiency Syndrome (UNAIDS) 2013 report depicts the HIV epidemic in Ghana to be a generalized epidemic with a prevalence of more than 1%. The HIV prevalence in Ghana is not generalized but varies with geographic regions, age and gender. Highest prevalence was recorded within 35-39 year age group with 43% prevalence in males and 57% in females. The following regions; Greater Accra, Western, Volta, Northern, Upper East and Upper West recorded the highest increase of prevalence in 2012. In the Northern region for example, service providers revealed an increase in young (15-30 years) nubile female head porters. The health facilities see a noticeable increase in these ladies with advanced HIV infection and subsequently dying from AIDS related complications (12).
Having spent a month working with Society for Women Living with AIDS in Africa (SWAA) in partnership with UNAIDS, I had the opportunity to visit 3 socio-economically deprived regions of Ghana. We visited some health facilities in rural areas of WA, Tamale and Bolgatanga all in the Northern region. The healthcare system in Ghana requires the patients to visit the Anti-retroviral Drugs (ARV) Center monthly for their ARV and a GHC5.00 surcharge. A recurring problem highlighted was the lengthy journey times in order to access treatment at the ARV centres in addition to the surcharge. On average, the closest ARV centres in these regions were over 5km away from their residences, which was a financial burden in terms of transport costs. This lack of remote access was identified as a leading cause of the increase in HIV-related morbidity and mortality especially among the women in the region. In addition to this, there was a lack of HIV testing commodities and a shortage of staff thus longer waiting periods for monitoring of CD4 counts. A lack thereof of viral load testing equipment and reagents as part of quality ARV service delivery was raised. As a result, critical steps must be taken to properly address this malaise.
WHO outlined the key components of a functional health system; they include the following: improving individual’s health, defending the population from factors of a threat to national health, protecting against financial consequences of ill health, providing equitable access to people centered care and involving people in the decision-making process affecting their health and healthcare system (4). Access to essential medical products and technologies is essential to a national health system as well as ensuring the health delivery systems are reliable and convenient.
Findings from research conducted by the International Finance Corporation – with help from McKinsey & Co – on the main problems in Africa’s healthcare system and possible solutions highlighted 5 imperative solutions, namely (1):
Developing mechanisms for creating and enforcing quality standards for health services and medical product manufacturing and distribution.
Including as many of the population in risk pooling programs.
Channeling a proportion of public and donor funds through the private sector.
Enacting local regulations that are more encouraging of the private health care sector.
Improving access to capital, including by increasing the ability of local financial institutions to support private healthcare enterprises.
This short brief and communication focuses on the 1st point for the various reasons; the medical product manufacturing and distribution has potential to be most profitable in the SSA, albeit not being exploited sufficiently. Across SSA, local pharmacies play a major role in subsidizing the hospitals and clinics’ financial income; for example there is a Kenyan outpatient clinic with up to 70% of its profit originating from their pharma department (1). Nigeria is a prime example whereby monopolies strive with one leading pharmaceutical manufacturer supplies to over 100 outsourced distributors out of a possible 724 medical licensed distributors. This highlights the market domination by a handful of companies and the need for development and diversification, as dependency on one source is risky. This lays emphasis on the need to improve and innovate medical product manufacturing and distribution of medication as well as healthcare services.
A general concept that eventually coined the term community based delivery (CBD) has shown success in various countries with different applications. The focus within this context is placed on the healthcare workers deployed by the government or non-governmental organizations (NGO) to deliver services to the community. This has addressed a major shortage of human resources within low and middle-income countries and improved the quality of the healthcare system. The deliveries of insecticide-treated nets in Kenya and preventive malaria treatment in Southern Malawi are a few examples where CBD has been a success. In community-based sites in Kenya, there was an increase in bed net ownership from 21% to 61.1%. In Southern Malawi, preventative malaria treatment coverage increased from 41.5% to 81.9% (5, 6). The results from this study showed a general increase in effectiveness of this delivery approach.
Innovative technologies and approaches will further effectuate the delivery of healthcare reforms. Bangladesh is reputed for being one of the first few developing countries to implement innovative technologies, policies and approaches towards improving their healthcare system. There has been a surging increase in government partnerships with local NGOs and institutional research to foster the development of innovative technologies, which are beneficial to the specific population. These techniques have seen the development of oral rehydration solutions and designing community based family planning programs (8).
South Africa is looked upon as a hub for life sciences innovation in SSA. It finances, encourages and fosters the development of its innovation industry revolving around existing research capabilities. The government funded and fostered the development of telemedicine in Tsilitwa, a suburb in the Eastern Cape of South Africa. The nearest hospital to Tsilitwa is 10 miles away without connecting roads. South Africa’s Center for Scientific and Industrial Research equipped Tsilitwa’s health centres with the necessary equipment to allow live feed and communication between the nurses at the clinic and doctors in the hospital. This clinic attends to about 10,000 patients monthly and has no doctors physically present. This demonstrates that technological innovation will go a long way in bolstering the healthcare system across the given population based on the common ills identified. This should thus result in higher attendance rates for patients, speed of patient dispatch by having the appropriate number of doctors on-site. In addition, the positive feedback loop this system creates extends far beyond the creation of the technologies but also education and job opportunities. On a larger scale, by creating a robust healthcare system characterised by sophisticated technology platforms, the population should progressively become self-sustainable with little or no reliance on foreign aid.
An estimated $1 billion allocated towards pharmaceutical production1 in SSA has over 70% concentrated in South Africa alone. Nigeria, Ghana and Kenya represent about 20% of this continental fund. Swipha, located in Nigeria could be used as a case study as a leading generics manufacturer with potential and room for growth. Bio24 is another example in Senegal of a growing diagnostic laboratory with services in high demand to health providers, research centers and the general public. The system offers opportunities to the population for novel approaches and solutions towards local health challenges.
While the evolving technology development increases, there is a vital need for government policies to be instated or reinforced to allow for the translation of the changes to be observed by and among the general public. This creates a strategy for the implications into human resources, pharmaceuticals, and technology infrastructure and service delivery placing relevant guidelines, plans and targets for subsequent implementation. Africa’s pharmaceutical industry rose from $4.7 billion in 2003 to $20.8 billion in 2013 and expected to climb to $3.3 trillion by 2020. The cumulative growth is a product of 10 countries (Algeria, Egypt, Kenya, Ivory Coast, Libya, Morocco, Nigeria, South Africa, Sudan and Tunisia) out of the 54 (11). This highlights the need for expansion and creation in the other 44 countries.
Taking into account the estimates projected for the next decade of investment into healthcare systems in Sub-Saharan Africa, creating research institutions for technological development and innovative delivery approaches, as a venture for investment, is absolutely vital. This takes CBD a step further by not only delivering services to the inhabitants but also creating an environment and providing a platform for social education, fostering innovation of technologies, ideas and novel approaches whereby the community at large can contribute to the development of a more sustainable healthcare system and alleviate dependency on foreign aid. The lack of on-going research detracts potential scientists in the diaspora from returning to their country of origin to pursue their careers as there is a feeling of reaching a “final ceiling” with no room for further progression. The lack of incentives further result in brain drain in Sub-Saharan Africa with only 3% of healthcare professionals and experts deployed to rural regions (1, 8).
The Trade-Related Aspects of Intellectual Property Rights (TRIPS) agreement supported by the Doha declaration reiterated; “it does not prevent members from taking measures to protect public health.” UNAIDS executive director, Michel Sidibé stated, “countries should not trade away the public health of their people for other trade gains” (9). This places a call on governments of SSA countries to take advantage of this agreement and invest in the local manufacture of essential drugs and encourage CBD. This entails interdisciplinary cooperation between different sectors including policy makers, research scientists, healthcare training personnel and economists directing the flow of funds into each project. There are high stakes involved including very high level of commitment from various parties but this is not insurmountable.
It is imperative that local governments in partnership with local NGOs and enthusiastic investors jointly address the issue of community based delivery services. Investments in essential medical products and technological research and development in local communities should be encouraged both financially as well as via widespread education as this creates a social village.
Full-text article previously published United Nations Peace & Progress : https://postgraduate.ias.unu.edu/upp/wp-content/uploads/2016/07/5_Zekeng_article.pdf
How can we concretely engage girls in Science-related fields of studies in Africa?
I believe there are a multitude of reasons that explain women’s underrepresentation in science in Sub-Saharan Africa..
Interviewed & published by Next Einstein Forum.
Next Einstein Forum: In 2016, the European Union selected you as Young Leader in recognition to your contribution in the field of science, notably in Africa. Could you tell us more about this and how you passed the so-called “glass ceiling”?
Elsa Zekeng: At the time of my selection I was doing my PhD in Infectious Diseases and Global Health at the University of Liverpool and was Co-Founder of an organization called the “Northwest Biotech Initiative”. The initiative aimed to equip scientists with skills and tools essential for career paths outside academia for example if they wanted to commercialize their research or go into industry or consulting. As well, and I suppose more interestingly, in 2015, during the biggest Ebola outbreak in West Africa, I deployed to Guinea with the World Health Organization (WHO). I spent six weeks at an Ebola Treatment Centre in Coyah testing patient and contacts’ samples for Malaria and Ebola. This was to support contact tracing and slow down the spread of the Ebola outbreak. I later received the ‘Ebola medal for service in West Africa’ from Her Majesty Queen Elizabeth, II from England.
I have been very fortunate, and have achieved a lot but I wouldn’t say I have passed the “glass-ceiling” as I still have a lot to achieve. Nonetheless, I attribute these achievements to several factors. My father consciously exposed me to a range of experiences from a very young age. He was and still is an absolute advocate on the importance of education and being able to achieve anything I set my mind to. My PhD supervisor played a role in this as he understood my goals, saw my potential and gave me the opportunity. Finally, the community of dedicated women in science from whom I have drawn strength at various points knowingly and unknowingly. I am aware I am very fortunate to have been able to pursue these opportunities and have a relentless support system.
What is the current landscape of gender equality in science, technology and innovation (STI) fields on the continent?
E.Z.: According the Lancet journal, when considering Science, Technology, Engineering and Mathematics (STEM), 53% of the world’s bachelor’s and master’s degree graduates and 43% of PhD graduates are women. However, only 28% of researchers are women in these fields and only 30% of women in higher education move into STEM-related roles. In Sub Saharan Africa, only 30% of researchers in all subject areas are women. Taking Cameroon as an example, in 2017, 20% of men enrolled in tertiary education whilst only 15% of women enrolled. Further, only 22% of Cameroonian researchers are female academics while 7% of female academics rank as full professor. An in-depth analysis showed that female scientists constituted lower ranks of the workforce with less responsibility, decision making and leadership opportunities.
What are the reasons that explain women’s underrepresentation in science in Sub-Saharan Africa?
E.Z.: I believe there are a multitude of reasons that explain women’s underrepresentation in science in Sub-Saharan Africa but I would like to focus on two specifically. The first is access and encouragement into STEM subjects at a young age. I believe culturally and socially, girls should not only have access to education in STEM subjects but also be encouraged to pursue these careers. STEM fields are already male dominated and may be intimidating for any young female with an interest in this. Girls should be encouraged to embrace the trial and error approach that science and technology demands. Therefore, building confidence and resilience is absolutely key.
An interesting observation was made when I was speaking on a panel at the Liverpool School of Tropical Medicine. Girls who attended all-girl schools at some point in their education attained higher levels in STEM fields. This was interesting to me as I went to an all-girl school for 7 years (Secondary school to High School). So, I thought and continuously think about it, could this be because we felt safer to keep trying in our formative years? That would be an interesting piece of research to carry out.
The second one is related to systemic and institutional gender biases (conscious and unconscious). We all have an unconscious bias. There are several types of these biases which infiltrate the world of work and affect how we interact and engage with people different from us. For example; “affinity bias” is where we gravitate to people like ourselves in appearance, beliefs and background. This is frequently seen in the recruitment processes. As stated above, STEM fields are generally male dominated. This leaves women interested in pursuing STEM careers at the mercy of biased policies, recruitment practices, progression opportunities, workplace culture and so much more. This is absolutely key as we could have a talent pipeline of promising, hardworking women with a desire to pursue careers in STEM. However, if met with obstacles that are beyond their control, such as a non-inclusive work environment, limited opportunities for progression, limited mentorship opportunities consistently, this would understandably frustrate even the brightest and most hardworking person.
How can we concretely engage girls in science-related fields of studies and careers in Africa? How can they overcome the barriers?
E.Z.: As mentioned above, engage with girls and encourage them into science-related fields from a very young age. Through after school activities, events that allow girls to engage with and talk to women in science at various career levels, building online safe spaces and community groups to continue this conversation. More importantly, making them aware of various job opportunities following science -related studies. It is very important to inform and educate girls and our society on job opportunities upon completion.
When families, friends and well-wishers are informed on the opportunities available, the girls build a safe support group that continuously encourage them to pursue this career. The public perception is frequently limited to think that following education in STEM subjects, the only career options are “medical doctor” or “engineering”. This is simply not the case as there so many more career paths available. Our governments and leaders should get more involved and invest in science and technology related careers whilst transmitting this information to girls from a young age and their families and well-wishers. This instills trust and a sense of direction and purpose to push on when the going gets tough.
How innovation can develop an environment in which more of girls and women engage in STI studies on the continent?
E.Z.: Technology decentralizes the process of learning and upskilling. It provides community groups the technical as well as the emotional support to grow and thrive in these spaces at an individual pace without external pressures or fears. It allows for collaboration and learning beyond geographical borders. It is crucial to build an ecosystem that supports the development of science and technology. We should also build technology that combats biases. I am a Co-Founder of a start-up called Jobseekrs. Jobseekrs mitigates unconscious bias at the sourcing and screening stage of recruitment. Jobseekrs is an AI powered interactive job site that matches candidates to job opportunities on two key factors, namely their competency to the job role and their culture-alignment with a company. Our machine learning algorithm combines the results from these two factors into a percentage fit score for each candidate. It presents these candidates to the employer anonymously only showing the percentage fit score for initial vetting; not their name, gender or any other thing that may cause a form of bias. Our mission is to give everyone an equal chance. This is the power of technology when used globally, to address systemic obstacles that have at one time, disadvantaged a particular set of people. Building more technology that combats inequalities will definitely increase and engage more girls and women in Science and Technology. It is worth noting that access to technology is still a privilege that needs to be further decentralised. Ensuring that everyone has unlimited access to technology at an affordable cost is essential to fully reap all the benefits of technology.
According to various experts, the promotion of local African languages is a key element to reduce the inequality access to new technologies on the continent. Do you agree? Why?
E.Z.: When considering barriers to entry for anything be it technology or even a new subject at school, language is first and foremost a priority. Ensuring that information and key concepts are shared in a way that is accessible and understood to all is absolutely fundamental. This is also applicable to accessing new technology. We have to ensure it is in a language that is understandable to all to use it, understand it and furthermore build and create it.
Depression in PhD Students & Youth
A doctorate in philosophy (PhD) is still one of the highest academic qualifications attainable.
I can hardly pin-point the start or trigger of my interest and passion for global health. I frequently refer to a point when I was about 7 where I witnessed the impact of my father’s work with HIV/AIDS on people in Cameroon (my home country). Or, to a point when I was 16 and I spent a week travelling to 3 of the most socio-economically deprived regions in Ghana visiting various Anti-retroviral (ART) centres with himself as UNAIDS country coordinator for Ghana alongside the country coordinator of Society of Women Living with AIDS in Africa (SWAA).
Currently in the final year of my PhD in infectious Disease and Global Health at the University of Liverpool, and the starting point on this journey seems quite distant and somewhat irrelevant. It is safe to say whatever it was, the yearning for more education and solutions is deep-seated, profound and constantly enlarging with time, experiences and the current social climate we live in.
The reminder of World Health Day flooded many themes to mind as I contemplated what to focus this article on. Upon further research and learning this year’s theme – “Depression – let’s talk about it”, I instantly found the theme I will go on to address.
Considering my background and current position, I will focus on mental health problems in PhD students and youth, as well as depression in people in low and middle income countries (specifically Sub-Saharan Africa). I must admit, when I initially thought of my areas of interest in health, mental health was seldom at the top of my list. This is therefore unchartered territory for me but one that has seized my attention and led me into another dimension on this journey and interest in global health.
Mental health problems in PhD students and youth
A doctorate in philosophy (PhD) is still one of the highest academic qualifications attainable. It is therefore interesting to note, a study based on 12 mental health symptoms showed 32% of PhD students are at risk of having or developing a common psychiatric disorder especially depression. Yet, national figures in the United Kingdom for example in 2012 showed approximately 1 in 500 individuals reporting a mental health problem to their university. The fear of stigma and adverse effects on a future career has led to a reluctance to seek help.
The number of new PhDs (recipients of doctorate degrees) grew from 158,000 in 2000 to 247,000 in 2012; an increase of 56%. This increase was accompanied by budget cuts and increased competition for research resources. The laws of mathematics and demand and supply will agree on the inability to marry the number of PhD students produced by various institutions, with future academic careers following research budget cuts.
What has become the “norm” is the idea of spending on average 4 years (in most European countries) doing a PhD with no job security or specific knowledge on how to navigate from point A (end of PhD) to point B (desired career). This effect has somewhat diluted the sense of achievement upon completion of a PhD into looking for the next best opportunity. This process is frequently accompanied by various stresses such as; fear of failure, funding running out, thesis writing and making future career decisions in a heavily saturated field. This situation is made furthermore difficult for international students contemplating future career options due to the sponsorship requirements for job hiring.
Highlighting this in PhD students doesn’t detract away from this as a phenomenon currently plaguing many youths in both the developed and developing world. In 2016, it was reported within the UK, drinking, smoking, drug taking and teen pregnancies are at their lowest but depression and anxiety have increased by 70% in the past 25 years in teenagers. The question stands, how has society managed to produce a generation with such prevalent mental health problems? While this could be attributed to a number of factors, I believe one of them is – uncertainty of the future.
Another article recently stated, Millenials are the most educated generation in U.S history but yet struggle to attain professional success. Realities are; 39% of people under 25 are unemployed or underemployed. There is an imbalance which needs to be addressed between the education system, skill set, job creation and thus professional success. It is the responsibility of the institutions and governments to create prosperity and ensure employment of youth and in the specific case of PhD students, balance the demand and supply in academia and in industry. These will go a long way to solve some mental health problems especially depression stemming from a job insecurity and other issues which go alongside this such as quality of life.
Depression in low and middle income countries (specifically Sub-Saharan Africa)
In Sub-Saharan Africa, depression is an important but frequently neglected public health problem exacerbated by different circumstances. The prevalence of depression in Sub-Saharan Africa (SSA) is at about 5.5% but in people living with HIV (PLHIV) it is about 8%. Some of the challenges faced include; coping with diagnosis, social rejection, co-existing poverty and relationship crises to name a few. Depression in post-natal mothers reports higher figures. A study carried out by the Harvard Chan School of Public Health highlighted a significantly higher level of maternal depression in low and middle income countries compared to higher income countries. Several risk factors include; partner violence, low maternal education attainment and socioeconomic status. The common thread amongst all the risk factors of depression regardless of the group examined at any one time is; socio economic status, lack of education and gender inequality. It is therefore no surprise that several factors which play crucial roles in prevention of depression include; alleviating poverty, improving education, reducing violence and gender equality. These factors all feed in one way or the other to the sustainable development goals (SDGs).
The SDGs have a duty to go beyond reducing poverty but also creating prosperity, to go beyond encouraging education but creating a society able to absorb and value this education, to go beyond motivating Youth but empowering and ensuring sustainability and continuity. As of 2015, unemployment rates in Africa compared to the rest of the world were 7.44% and 6.00% respectively. The total youth unemployment reached 30.4% in North Africa and 48.1% in Sub-Saharan Africa. In Sub-Saharan Africa, 61.4% of youth lack the level of education expected to make them productive on the job.4 These figures are at an all time high, it is therefore unpractical to think there is no direct link between education/employment and the level of health. The expectations placed on understanding the need for access to healthcare and obtaining frequent tests for sexually transmitted diseases are unfair with increase unemployment, lack of security and somewhat limited knowledge on disease transmission at all levels within the community. It is impractical to expect an individual to consider long-term effects (such as mental health in this case) when the short-term needs (food and shelter) are not met via high unemployment rates and low socioeconomic status . In order to facilitate an improvement in the status quo, a positive change in the employment/education landscape alongside a change in the health sector is needed.